
Written by:
Courtney Battaglia BSN RN
February 15, 2026
Arterial vs. Venous Blood Clots: What’s the Difference?
When people hear the term “blood clot,” it can sound like just one condition. In reality, blood clots can form in different parts of the body and affect health in different ways. For American Heart Month in February and Blood Clot Awareness Month in March, we’re highlighting the close connection between blood clots and heart health.
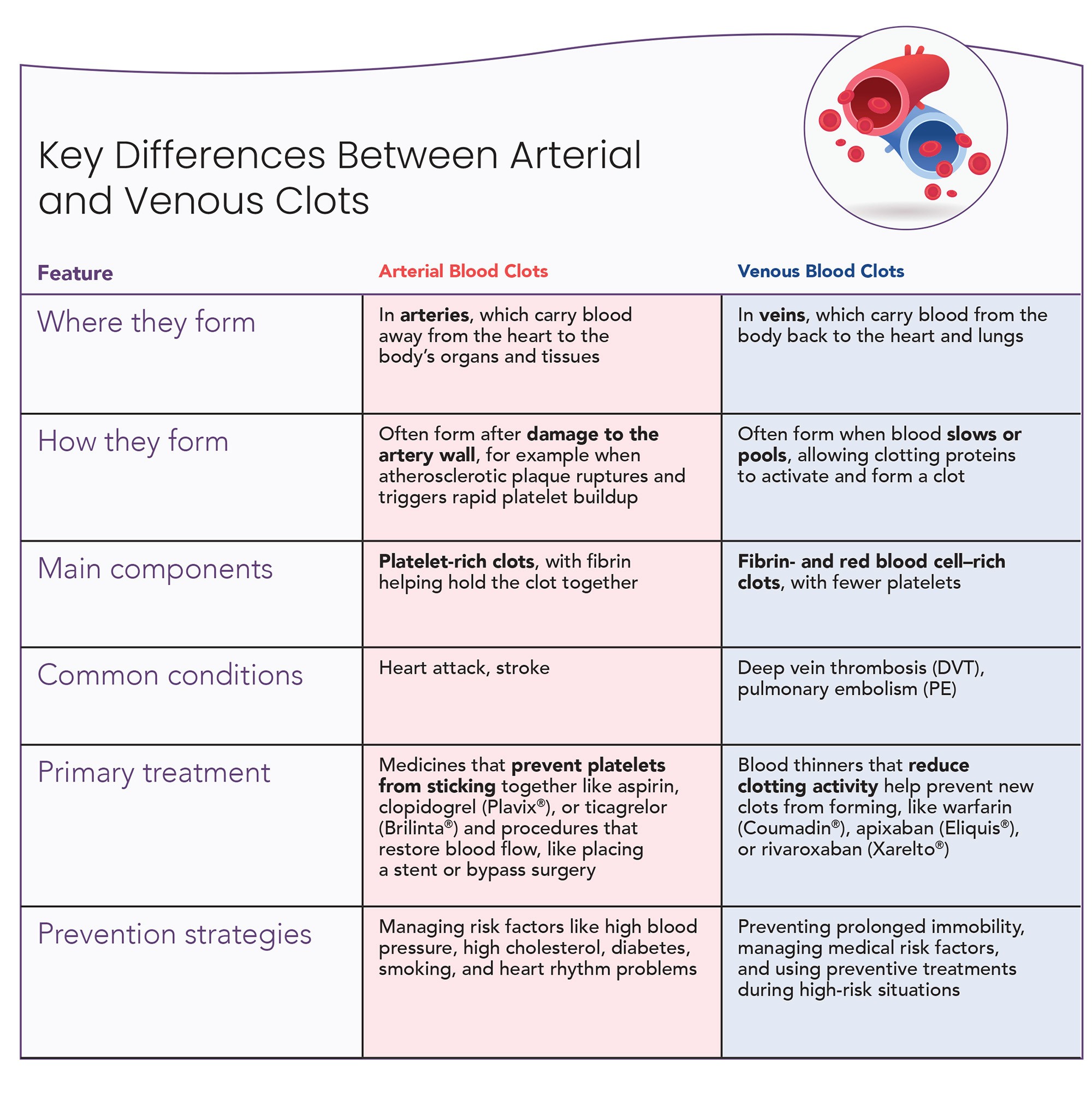
Some blood clots form in arteries, while others form in veins. Although both involve the circulatory system, they tend to develop differently and are linked to different health problems, with some overlap in risk factors.
Understanding the difference between arterial and venous blood clots can help explain why conditions like heart attack and stroke are different from deep vein thrombosis (DVT) and pulmonary embolism (PE).
What Are Arterial Blood Clots?
Arterial blood clots form in arteries, the blood vessels that carry blood away from the heart to the rest of the body, including the heart muscle and brain. These clots develop in areas where blood is usually moving quickly and under higher pressure.
Arterial clots often develop after damage to the inner lining of an artery. A common trigger is the rupture of atherosclerotic plaque, fatty buildup inside the artery wall. When plaque ruptures, it exposes the vessel wall and causes platelets to rapidly clump together and form a clot, even while blood continues to flow.
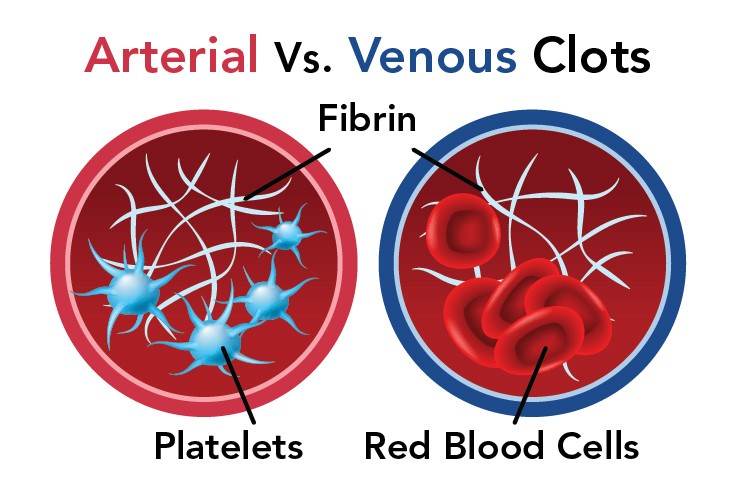
Arterial clots are rich in platelets and fibrin. These clots play a central role in heart attacks and ischemic strokes, which occur when blood flow to the heart or brain is suddenly blocked.
Certain heart conditions can also increase the risk of arterial clots. For example, atrial fibrillation can cause blood to pool inside the heart, where a clot may form and later travel to the brain, leading to a stroke. Long-standing risk factors like high blood pressure, diabetes, high cholesterol, and smoking further damages blood vessels and promotes plaque buildup over time.
What Are Venous Blood Clots?
Venous blood clots form in veins, the blood vessels that carry blood back to the heart and lungs. They usually develop when blood flow slows or pools, most often in the deep veins of the legs or pelvis. When a clot forms in these veins, it's called a DVT. When part of the clot breaks loose and travels to the lungs, it's called a PE. Together, DVT and PE are referred to as venous thromboembolism (VTE).
When a clot forms in a vein, it can block blood flow and cause symptoms like swelling or pain. Venous clots are rich in fibrin and red blood cells, with fewer platelets than arterial clots. This composition is linked to slower-moving blood and helps explain why venous clots often form during periods of limited movement. Things like prolonged immobility, recent surgery, illness, or certain medical conditions can increase the risk of venous blood clots.
What This Means for You
Understanding whether you’ve had an arterial or venous clot can help you:
Better understand your diagnosis
Ask more informed questions
Follow the prevention or treatment plan that’s right for you
Arterial and venous blood clots develop through different processes and affect the body in different ways. Recognizing those differences helps explain why conditions like heart attack, stroke, DVT, and PE are related—but not the same.
────────
What a Calcium Score Can Tell You About Heart Health
Plaque often starts building up inside the arteries years before symptoms show up. Changes within arterial walls can quietly shape heart health over time, which is why clinicians use various tools to understand risk better.
Plaque and the Arteries
Plaque is a mix of fat, cholesterol, immune cells, and other materials that slowly build up inside the walls of arteries. As plaque forms, immune cells absorb fat and become trapped in the vessel wall, which contributes to ongoing inflammation. Eventually, a fibrous, hardened layer can form over the plaque, covering the softer material underneath.
Arterial plaque often goes unnoticed because arteries can stretch outward as plaque builds up within the vessel wall. This process, called positive remodeling, allows plaque to grow while preserving blood flow. As a result, symptoms may not appear until plaque becomes more extensive.
Factors That Affect Arterial Health
Many of the factors that affect arterial health are well known, but seeing them together can help put calcium scores into context.
Modifiable (Things you can change) | Non-modifiable (Things you can't change) |
|---|---|
Smoking | Age |
Cholesterol | Sex |
High blood pressure | Family History |
Diabetes |
What Is a Calcium Score?
A calcium score, also known as a coronary artery calcium (CAC) score, is a measurement of how much calcified plaque is present in the arteries that supply blood to the heart. The test is performed using a specialized CT scan (a type of imaging test that takes detailed pictures of the heart). It's quick, painless, and noninvasive. You lie on a table while images of your heart are taken, usually in just a few minutes. No contrast dye or injections are needed, and you can return to normal activities right after the scan.
Calcium deposits in arterial walls are a sign of plaque buildup. Higher calcium scores mean more plaque in the arteries and a greater risk of heart disease. A score of zero means no calcified plaque was seen at the time of the scan.

What a Calcium Score Can—and Can’t—Tell You
A calcium score can help estimate your risk of atherosclerotic cardiovascular events, like a heart attack or stroke. This information can be useful when a clinician is assessing your overall heart disease risk—especially when that risk isn’t already clear. It can also help guide conversations about long-term heart health and which prevention strategies may be most helpful.
A calcium score doesn’t capture all types of plaque. Softer, non-calcified plaque can still be present and may still carry risk, even when the score is zero. Because of this, a calcium score can’t rule out coronary artery disease (CAD) on its own. If you have symptoms or are at higher risk, your clinician may still recommend further evaluation. A calcium score also doesn’t show how narrow an artery is or whether a blockage is limiting blood flow.
Should You Discuss a Calcium Score with Your Clinician?
A calcium score isn’t used for everyone. It’s most often discussed when your heart disease risk isn’t already clear and additional information could help guide next steps.
A calcium score may be discussed if you:
Are between ages 40–79 and have borderline or intermediate heart disease risk, especially when it’s unclear whether starting a statin makes sense
Are at lower calculated risk but have additional factors that raise concern about underlying plaque
A calcium score is generally not used if you:
Have known cardiovascular disease, like a prior heart attack or stent
Are already taking statins
Clearly need statin therapy regardless of the result, since the score would not change management
How Calcium Scores Fit Into the Bigger Picture
A calcium score is one tool clinicians may use to better understand heart and vascular health risk. It’s not a standalone diagnostic test, but it can help guide conversations about prevention and long-term heart health.
────────
Board Member Spotlight: Meet the People Behind the Work
At VLN, our work is guided by board members who bring deep clinical and research expertise to vascular health education.
In this opening installment of our Board Member Spotlight, we’re introducing the people helping guide VLN’s work. This issue features Christian Ruff, President of VLN, Director of General Cardiology at Brigham and Women’s Hospital, Associate Professor of Medicine at Harvard Medical School, and a leading clinical trialist with the TIMI Study Group. His work focuses on cardiovascular disease, blood clots, and stroke prevention.

What drew you to your work in this field?
Dr. Ruff's path into cardiology was shaped early by personal experience. His twin sister was born with a congenital heart defect and underwent heart surgery as a child. That experience had a lasting impact on him and his family. “Time stands still when a family member, a loved one, has a serious medical condition,” he said, reflecting on how grateful they were for the care, reassurance, and compassion shown by the healthcare team during an incredibly stressful time. Later, when his grandmother developed Alzheimer’s disease, he again saw how meaningful compassion and support can be—especially in helping patients and families cope with a difficult illness and diagnosis.
Together, these experiences shaped his desire to go into medicine, and particularly academic medicine, where he could care for patients while also being involved in education.
In your work, what do you think patients often misunderstand—or don’t hear enough about—when it comes to their condition or vascular health in general?
One of the most common misunderstandings Dr. Ruff sees is how much control patients actually have over their health. After a diagnosis, many people feel powerless and assume their outcomes depend entirely on medications or procedures. While treatments matter, he emphasized that daily habits play a major role in long-term outcomes. “What people do in their day-to-day lives makes a huge difference,” he said, pointing to physical activity, lifestyle choices, and behaviors that can worsen or improve symptoms.
He also noted that medicine often focuses more on treating disease than preventing it. Maintaining vascular health early—long before a diagnosis appears—is often far more impactful than managing disease later. “We do a good job managing disease,” he said, “but we have to do a much better job talking about prevention and maintaining health.”
What’s one thing you wish every patient felt more comfortable asking about during their care?
Dr. Ruff encourages patients to be active participants in their care. Medical visits can feel rushed or intimidating, and patients may hesitate to speak up when they don’t understand something or feel unsure about a recommendation. “It’s your body,” he said. “You have to be comfortable with every decision that’s made.” He believes patients should feel empowered to ask why a treatment is recommended, what alternatives exist, and how different options align with their goals and concerns.
He also emphasized that healthcare should be a partnership. Clinicians bring medical expertise, but patients bring lived experience—and both are essential in making informed decisions.
Is there a habit or practice you often talk about with patients that you also try to follow yourself?
Dr. Ruff shared that he’s become more intentional about practicing the same habits he encourages in patients. Earlier in his career, busy schedules sometimes made consistency difficult. Now, he prioritizes routines—taking medications regularly, staying hydrated, exercising, and paying closer attention to nutrition. He described becoming more mindful of sodium intake by reading food labels and choosing minimally processed foods, noting that he was surprised by how much sodium he had been consuming before. Following this advice himself has given him a deeper appreciation for how challenging lifestyle changes can be—and how important consistency really is.
Why was it important for you to be involved with Vasculearn Network?
For Dr. Ruff, education is one of the biggest gaps in healthcare today. Despite advances in science and treatment, patients and clinicians alike are often overwhelmed by information and unsure what sources to trust. “There’s so much noise out there,” he said. “Physicians and patients are overwhelmed, and it’s hard to figure out what’s real.” He emphasized that education is often divided. “Healthcare is a therapeutic relationship between patients, their caregivers, and healthcare providers,” he said. “But so much of the education happens in two separate domains, and that leads to gaps in communication and understanding.”
He values VLN’s commitment to expert-curated, unbiased information and to building a supportive community. Creating “a safe home of valuable information” helps people feel more confident, informed, and less alone as they navigate complex vascular conditions.
────────
Upcoming Patient Events
Our groups are free to join and start at 7:00 pm EST.
Blood Clot Support Group (Monthly)
Hosted by Joelle Hochman, RRT, Chair of Patient Engagement & Education
Blood Clot Support Groups are peer-to-peer conversations for people who have experienced a blood clot. These sessions offer a space to ask questions, share real-life experiences, exchange practical tips, and connect with others who understand the emotional side of living with a blood clot.
• • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • February 19 • March 19 • April 16
Long-PE and CTEPH Support Group (Every other month)
Have you or someone you care for experienced a pulmonary embolism (PE)? VLN offers a dedicated support group for patients with post-PE syndrome and CTEPH (Chronic Thromboembolic Pulmonary Hypertension). This group provides a safe space to connect with others, receive support, and learn more about managing life after PE.
• • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • March 12
Spanish-Speaking Vascular Health Group (Quarterly)
Chronic pelvic pain can be confusing, especially when tests don’t provide clear answers. In this live session, Dr. Alfonso Tafur and Dr. Nathalia Cardoso will discuss how vein-related conditions can sometimes contribute to pelvic pain. They’ll cover common symptoms, why diagnosis can be challenging, and questions patients can ask when seeking care.
El dolor pélvico crónico puede ser confuso, especialmente cuando los estudios no dan respuestas claras. En esta sesión en vivo, el Alfonso Tafur y la Nathalia Cardoso hablarán sobre cómo los problemas relacionados con las venas pueden, en algunos casos, contribuir al dolor pélvico. Se abordarán síntomas comunes, por qué el diagnóstico puede ser difícil y qué preguntas pueden hacer los pacientes al buscar atención.
• • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • February 17
Join us to learn more about your heart, circulation, and clot-related conditions at VLN’s Ask the Expert sessions. These live Q&As with trusted specialists offer clear answers and helpful guidance.
Here's what's coming next:
February 25: Do I Need Thrombophilia Testing? Understanding Blood Clotting Disorders with Dr. Behnood Bikdeli
April 8: Heart and Stroke Prevention: Beyond Blood Thinners with Dr. Heather Johnson
Prefer to read or print?
If you’d like to read this month’s edition of The Beat offline, or keep a copy for later, you can download the full PDF version ->



