Last updated on
What is Atrial Fibrillation?
Atrial fibrillation (Afib) occurs when the electrical impulses that power the heart are uneven, causing the heart to beat irregularly. A heart with Afib works harder but pumps less blood. Blood can then pool in the atria, leading to possible stroke.
Who’s at risk?
Afib is a common condition that affects at least 2.3 million adults in the United States. It primarily develops in people over the age of 65. Patients with high blood pressure and heart disease, and those born with heart defects, have a greater risk of developing Afib.
Other risk factors include:
- Lung disease, such as chronic obstructive pulmonary disease (COPD)
- Diabetes
- Sleep apnea
- Inflammation around the heart
- Overactive thyroid
- Metabolic syndrome (obesity and diabetes)
- Alcohol abuse
What are the signs and symptoms of Afib?
- Heart palpitations
- Rapid irregular heart rate
- Low blood pressure
- Chest pain
- Shortness of breath
- Feeling light-headed or dizzy
- Weakness
- Fatigue (tiredness)
If you experience any of these symptoms, you should seek medical attention.
How is Afib diagnosed?
Diagnostic testing may include:
- An electrocardiogram (ECG)
- Wearing a Holter monitor, mobile cardiac monitor, or other type of event recorder
- An echocardiogram (echo)
- A transthoracic echocardiogram (TTE)
- A transesophageal echocardiogram (TEE)
- Cardiac computerized tomography (CT)
- Magnetic resonance imaging (MRI)
Stroke risk
Patients with Afib are at risk of developing blood clots in the heart, which can lead to ischemic stroke – a stroke caused by a clot blocking blood flow to the brain. About 15% of strokes can be attributed to Afib, and these strokes tend to be more devastating than other types of strokes. Importantly, women with Afib have an increased risk of stroke compared to men and are also more likely to suffer more debilitating strokes. The good news is that 80% of all Afib-related strokes are preventable with anticoagulant therapy.
Anticoagulant drugs, also known as blood thinners, can prevent blood clots from forming and are commonly used in patients with Afib – but you need to know your stroke risk first before starting anticoagulation. Healthcare providers traditionally used a risk scoring system called the CHADS2 score to determine if a patient with Afib had a low, intermediate, or high stroke risk. That risk score has since been refined. Providers now frequently use the CHA2DS2-VASc score to calculate stroke risk in patients with Afib.
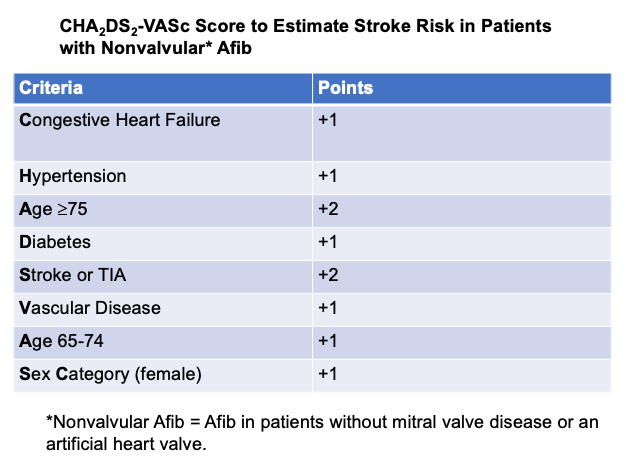
Providers will often prescribe anticoagulation if a patient scores a 2 or higher.
The CHA2DS2-VASc risk calculator can be found here.



