Thrombosis is the abnormal formation of a blood clot inside a blood vessel. Healthcare professionals may also call it a thrombus. Thrombosis prevents blood from flowing through the circulatory system. Without blood flow, tissues and essential organs, like the heart, can’t get enough nutrients.
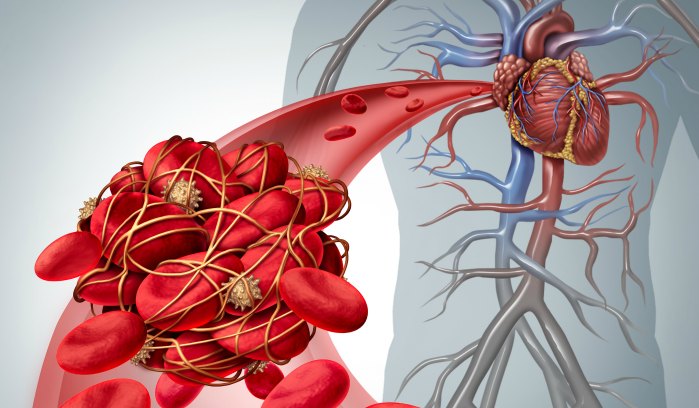
Blood clots that form and stay in place in the vein are called thrombi. When the blood clot detaches and travels through the bloodstream, it’s called an embolus. Thrombosis can develop in the arteries or the veins. Treatment will depend on the type, severity, and location of the clot within your body.
What Causes Thrombosis?
Blood clotting, or coagulation, is the body’s first line of defense against bleeding. Your body activates a clotting system when a blood vessel is injured, like from a cut. This clotting system forms a “plug” over the injury to prevent further bleeding. After the injury has healed, your body usually breaks down the clot. But sometimes, the clot fails to break down.
Blood clots can also form for reasons other than blood vessel injury. Certain health conditions, medications, or other medical treatments can cause blood to become too thick, increasing the chances of clotting. If blood flow is too slow because of lack of movement, blood can pool or rest in place. Blood that sits in one place for too long, tends to clot.
Types of thrombosis:
There are two main types of thrombosis.
- Arterial thrombosis: Refers to a blood clot that blocks an artery. Arteries carry blood away from the heart to other parts of the body. Arterial blood clots can block blood flow to the heart and brain. Blood clots in these areas can cause heart attacks or strokes.
- Venous thrombosis: Also known as venous thromboembolism or VTE, this type of clot happens in the vein. Veins carry blood from other parts of the body back to the heart. VTE is a condition that includes deep vein thrombosis (DVT) and pulmonary embolism (PE).
Thrombosis Risk Factors
Some people are more likely to develop thrombosis. Risk factors that can increase the chances of thrombosis include
- Surgery
- Obesity
- Smoking
- Diabetes
- Infections
- Pregnancy
- Major trauma
- Atrial fibrillation
- Family history of clots
- Limited physical activity
- Cancer and chemotherapy
- Inflammatory or autoimmune disease
- Genetic or acquired clotting disorders
- Plaque build-up in arteries or atherosclerosis
- Estrogen-containing birth control pills and hormone replacement therapies
Can blood clots be dissolved or removed?
The safest way to dissolve a clot is by allowing your body to dissolve it naturally. This process can take weeks to years, but some blood clots won’t go away without medical treatment. The type of blood clot and its location and severity will determine what kind of treatment you get. Treating blood clots may involve:
- Thrombolytics: Thrombolytics are medications given through an intravenous (IV) catheter in your arm. These medications dissolve the clot, allowing blood to flow.
- Catheter-directed thrombolysis: This procedure involves placing a catheter near the clot. Thrombolytic medications are then given directly to the clot.
- Surgery: A thrombectomy is a surgical procedure to remove clots from strokes, heart attacks, or pulmonary embolisms.
Anti-clotting medicines (called blood thinners or anticoagulants) decrease the blood’s ability to clot but increase the risk of excessive bleeding. Your healthcare team will need to monitor how your body responds to these medications.
What are the risks of blood clots recurring?
The chances of a recurrent blood clot depend on the circumstances leading up to the first clot. For example, if the blood clot occurred as a result of surgery or trauma, then the chances of re-occurrence is relatively low. On the other hand, for people who developed unprovoked blood clots and have stopped treatment after 6 months, the chance of recurrence is approximately 20% in the first 4 years and roughly 30% after 10 years.
What are the risks of taking an anticoagulant (blood thinner)?
Anticoagulants decrease the blood’s ability to clot. All anticoagulant medications increase the risk of excessive bleeding. Signs of excessive bleeding can include prolonged nose bleeds, severe bruising, bleeding gums, vomiting, or coughing up blood. Women may have heavy menstrual bleeding.
Patients who take blood thinners should seek medical attention immediately if they experience:
- Head trauma
- A major accident, such as a car accident
- Unstoppable or prolonged bleeding
Blood thinners are essential to treat blood clots. You shouldn’t stop taking them unless instructed by a healthcare professional. Speak with your clinician or a pharmacist if you have any concerns about taking a blood thinner – or if you have difficulty affording your medication.
Recently Diagnosed?
Interested in learning more about diagnosis or joining a patient support group? Check out some of our resources!
References
Ashorobi D, Ameer MA, Fernandez R. Thrombosis. In: StatPearls. StatPearls Publishing; 2024. Accessed on June 6, 2024.
Baig MU, BJ. Thrombolytic therapy. In: StatPearls. StatPearls Publishing; 2024. Accessed on June 5, 2024.
Blood Clots. American Society of Hematology. Accessed on June 5, 2024. https://www.hematology.org/education/patients/blood-clots
Blood Clots. Medlineplus.gov. Accessed June 5, 2024. https://medlineplus.gov/bloodclots.html
Centers for Disease Control and Prevention. Data and Statistics on Venous Thromboembolism. Venous Thromboembolism (Blood Clots). Published on May 15, 2024. https://www.cdc.gov/blood-clots/data-research/facts-stats/index.html
Mathews S, De Jesus O. Thrombectomy. In: StatPearls. StatPearls Publishing; 2024. Accessed on June 5, 2024.
Mount HR, Rich M, Putnam MS. Recurrent venous thromboembolism. American Family Physician. 2022;105(4):377-385.
The basics of blood clots: What you need to know. NIH MedlinePlus Magazine. Accessed on June 6, 2024. https://magazine.medlineplus.gov/article/the-basics-of-blood-clots-what-you-need-to-know