Read commonly asked questions about life after a blood clot in our patient content series, Is This Normal?!
Want to stay up to date? Check out our latest content on instagram and facebook, or subscribe to our e-newsletter for updates & articles about blood clots!
NOTE: This content is meant to be a guide only. Please contact your doctor with any questions or concerns.
Table of Contents
- Is it normal to have a Deep Vein Thrombosis or Pulmonary Embolism?
- Is it normal to have an unprovoked blood clot?
- Is it normal to feel anxious right after being diagnosed with a blood clot?
- Is it normal to have a PE without any evidence of a DVT?
- Is it normal to feel chest pain after having a pulmonary embolism?
- Is it normal for lung capacity to take a long time to return after PE?
- Is it normal to feel worried about having another blood clot in the future?
- Is it normal to not return to previous exercise levels many months after my blood clot?
- Is it normal to have a heavy period while on a blood thinner?
- Is it normal to bruise more when on a blood thinner?
- Is it normal to have residual trauma even months after a blood clot?
- Is it normal to have residual clot symptoms after a clot has gone away?
- Is it normal to still feel a blood clot under my skin after being told it’s gone away?
- Is it normal to taste a little blood after brushing teeth if I’m on a blood thinner?
- Is it normal to feel cold while on a blood thinner?
- Is it normal to experience some hair loss while on a blood thinner?
- Is it normal for my heartbeat to sound louder when I’m on a blood thinner?
- Is it normal to have changes in vision after starting a blood thinner?
- Is it normal to struggle to sleep after being put on a blood thinner?
- Is it normal to have a higher blood pressure while on blood thinners?
- Is it normal to be taken off of blood thinners after 3-6 months?
- Is it normal to be afraid of coming off of a blood thinner?
Is it normal to have a Deep Vein Thrombosis or Pulmonary Embolism?

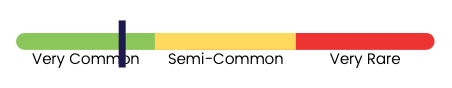
No, this is not usually considered “normal,” but it is not rare. The American Heart Association estimates about 1 million people in the US have a DVT or PE each year. While having a DVT or PE is not common enough to be considered “normal,”it is not rare to have a blood clot. Risk factors, such as immobility, inflammation, or smoking, may increase your risk of having a DVT or PE.
Is it normal to have an unprovoked blood clot?

No, this is not usually considered normal. Blood clots typically don’t form spontaneously, though it can sometimes be hard to determine why they formed. Genetics, medications, and medical conditions can increase the risk of clots. If a person has an unprovoked clot, they should be evaluated by their physician to determine further workup and treatment.
Is it normal to feel anxious right after being diagnosed with a blood clot?

Yes, this is normal. Many patients have only ever heard about blood clots in someone who has died or someone who had a stroke or heart attack. Additionally, knowing that you had the blood clot for a while, without being aware, can make you anxious. Finding a health professional to speak with can help calm your fears.
Is it normal to have a PE without any evidence of a DVT?

Yes, this is normal. Although many PEs originate from DVTs, it is not uncommon to diagnose someone with a PE and not find evidence of DVT. Whether or not a DVT is found when you are diagnosed with PE will not typically change the management of PE.
Is it normal to feel chest pain after having a pulmonary embolism?
Yes, this is normal. The pain caused by pulmonary embolism is typically sharp, feels worse when breathing in, and is accompanied by shortness of breath. It may last several days or longer (occasionally even a few weeks), but it eventually resolves. If you are experiencing chest pain for months after having a pulmonary embolism, please call your doctor.
Is it normal for lung capacity to take a long time to return after PE?
No, this is not usually considered normal. Your actual lung capacity (the amount of air your lungs can physically hold) is not affected by a PE, but it can take months to feel like you can take full, deep, breaths. Typically, if you are in good health, you should be able to return to “normal” deep breathing within 3 months. Exercise such as walking or swimming can help encourage faster recovery.
Is it normal to feel worried about having another blood clot in the future?

Yes, this is normal. Being diagnosed with a blood clot can be traumatic, so it’s natural to be afraid of having more clots. Any symptom that reminds you of the blood clot can trigger anxiety. If you find yourself worrying about new blood clots all the time, or if this worry prevents you from participating in normal activities or work, please seek help in the form of mindfulness activities, peer support groups, or counseling.
Is it normal to not return to previous exercise levels many months after my blood clot?

No, this is not usually considered normal. Typically, healthy patients should be able to return to their regular exercise habits within 3 months after having a blood clot. If you find it taking longer, you may have developed post-pulmonary embolism syndrome. This is not a well-characterized condition. However, patients with a possible diagnosis should see a specialist for evaluation and treatment.
Is it normal to have a heavy period while on a blood thinner?

Yes, this is normal. Blood thinners can lead to heavier and more exhaustive menstruation – and can sometimes even cause an iron deficiency. Speak with your doctor if you have questions about your blood thinner regimen and your period. If you take a blood thinner, staying hydrated, regulating iron levels, and taking a pain reliever like can help mitigate symptoms.
Is it normal to bruise more when on a blood thinner?

Yes, this is normal. Often patients on a blood thinner will bruise more often or more easily than before the blood thinner. If you have a bruise, aim to ice the area for the first 48 hours to decrease swelling and contact your doctor if it worsens or lasts more than 2 weeks.
Is it normal to have residual trauma even months after a blood clot?
Yes, this is normal. Many patients find a blood clot to be traumatic, especially if they were otherwise healthy. Being diagnosed with a clot can feel scary and life-changing. You can address trauma by reaching out to peers and talking with other people who have gone through the same thing. Don’t be afraid to discuss how you feel with your specialist or family physician. There is help available.
Is it normal to have residual clot symptoms after a clot has gone away?

Yes, this is normal. The most important part of managing someone diagnosed with a clot is preventing another clot from forming. Although a blood clot can resolve over time (at least partially), it’s not uncommon for symptoms to persist. Your physician can help prescribe treatments to alleviate the symptoms and often, symptoms improve over time.
Is it normal to still feel a blood clot under my skin after being told it’s gone away?
No, this is not usually considered normal. After a blood clot has dissolved, you should not be able to feel the clot anymore. However, if you start a blood thinner after 3 weeks of having a clot, you may have internal scarring from where the clot formed which may feel like a clot and often won’t go away. Being on a blood thinner only prevents new clots from forming – it does not prevent internal scarring from occurring.
Is it normal to taste a little blood after brushing teeth if I’m on a blood thinner?

Yes, this is normal. Some blood thinners may cause gums to bleed a bit. Brushing and flossing teeth can irritate gums, causing small tears or ruptures. This typically isn’t a big deal, and bleeding should stop pretty quickly. To alleviate pain, dissolve a little salt in warm water, swish for 30 seconds and spit to reduce swollen gums. Alternatively, steep a black tea bag in boiling water, allow it to cool, and place it on bleeding gums for a few minutes to help.
Is it normal to feel cold while on a blood thinner?

Yes, this is normal. Feeling cold is a listed side effect of warfarin, and something many patients on other blood thinners report. Your physician may refer to this as paresthesia,a burning, prickling, or cold sensation that’s felt in the hands, arms, legs, or feet (but may also occur in other body areas).
Is it normal to experience some hair loss while on a blood thinner?

Yes, this is normal. Hair loss happens primarily to patients on warfarin or heparin, and has been reported infrequently with apixaban, dabigatran, and rivaroxaban. Hair loss is often due to nutrient deficiencies, stress, or genetics. Aim to eat a balanced diet (including omega 3 & 6) with antioxidants, which can help promote hair growth.
Is it normal for my heartbeat to sound louder when I’m on a blood thinner?
No, this is not usually considered normal. If you are continuously hearing a louder-than-usual heartbeat, you may want to contact your doctor or ask to have an EKG or chest X-ray.
Is it normal to have changes in vision after starting a blood thinner?
No, this is not usually considered normal. Blood thinners should not cause blurriness or other changes to your vision. Please contact your doctor if you find that your vision is changing.
Is it normal to struggle to sleep after being put on a blood thinner?

No, this is not usually considered normal. A blood thinner should not cause insomnia, though sleep disruptions may stem from anxiety over having had a clot. Sometimes limiting caffeine or alcohol, or having conversation with your doctor about ways to improve your sleep, can help.
Is it normal to have a higher blood pressure while on blood thinners?
No, this is not usually considered normal. Blood thinners at conventional doses don’t impact blood pressure. Although your blood will take longer to clot when you’re on a blood thinner, this doesn’t increase or decrease blood pressure. Blood pressure that’s high for other reasons can increase the risk of bleeding, so it’s important to work with your physician control blood pressure.
Is it normal to be taken off of blood thinners after 3-6 months?
Yes, this is normal in many cases. Taking blood thinners (on time, without missing doses) protects new blood clots from forming. However, blood thinners can also cause bleeding problems. After 3-6 months of treatment and a discussion about your options and clot risk, your physician may advise that you stop taking blood thinners if the risk of having another blood clot is very low.
Is it normal to be afraid of coming off of a blood thinner?
Yes, this is normal. While some patients embrace coming off of a blood thinner (hello contact sports!), many are afraid to come off and risk having another clot. If this is a concern for you, voice your concern to your care team to find the right balance of and timeline for blood thinner use or discontinuation.
Have an “Is this normal” question you’d like to see featured? Send us an email with the subject line “Is This Normal” and we’ll add your question to the queue!