Last updated on
Physical Therapy: A Role in Blood Clot Management?
We often hear that physical therapy (PT) helps patients get back on their feet after an injury, surgery, stroke, or other medical issue. Physical therapists (PTs) can also play an important role in identifying signs and symptoms of a potential blood clot and in helping patients recover from clots. To learn how PTs can help with blood clot prevention and management, we turned to Dr. Ellen Hillegass, who specializes in PT for the heart and lungs (also known as cardiopulmonary PT). Dr. Hillegass is an Adjunct Professor at Mercer University in Atlanta, GA.
THE CRITICAL ROLE OF PTS
According to Dr. Hillegass, the core focus of PT is to help patients, including those who have had a blood clot, to get moving as quickly and safely as possible. “Our big thing is to get people mobile to prevent them from getting clots,” says Dr. Hillegass.
“If a patient has had a blood clot, then our role is first to identify when it’s safe to get up and be mobile, and then to teach them about signs and symptoms that are abnormal.”
PTs are often brought in to help patients get back to their activities of daily living shortly after an injury or surgical procedure – a critical time in a patient’s recovery. According to Dr. Hillegass, the first 28 days on average is when medical teams often see first-time or recurrent blood clots (patients may be most vulnerable to blood clots 28 days after an orthopedic surgery; for heart or chest surgery, this time window may be shorter). Patients who are discharged from the hospital to a rehab facility or to home care after surgery will typically see a PT several times a week and can be routinely assessed for risk factors for blood clots.
“We PTs are often the first ones to pick up on signs or symptoms of a blood clot because we are trying to help make patients more mobile, and we may observe that a patient has signs or symptoms of a blood clot that would prevent them from being mobile,” says Dr. Hillegass. “We are seeing more clots in the home setting these days because people in this 28- day period are a little mobile but maybe not enough to get the circulatory system moving sufficiently.”
BLOOD CLOT RISK
Surgery is only one risk factor for a clot. Other factors may include obesity, diabetes, smoking, or even a change in the use of a blood thinner medication. Pregnancy or hormone therapies containing estrogen (for example, some birth control pills) can also increase the chance of a blood clot. Patients with cancer are at a higher risk for developing clots, as both cancer itself and some chemotherapy treatments increase blood clot risk.
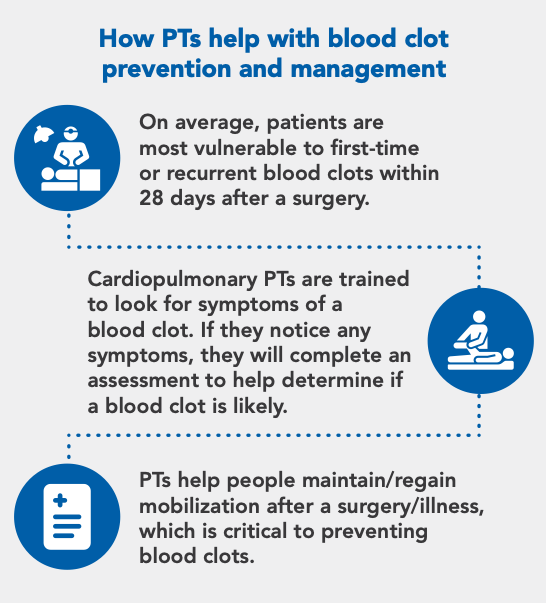
If a PT sees symptoms of a blood clot (such as pain or swelling in the leg or unexplained shortness of breath), they may use a risk assessment tool to help determine if a blood clot is likely. The assessment can be completed via a smartphone app or by paper and pencil. “The American Physical Therapy Association is working with a group called Guideline Central to develop apps and pocket guides that will help clinicians assess a patient’s risk for having a blood clot,” says Dr. Hillegass. “These tools allow PTs to input symptoms and other factors, like whether a patient is a smoker, if the patient has reduced mobility for more than three days, if they are obese, etc.” Depending on the results of the assessment, the PT might refer a patient for further testing. Dr. Hillegass adds that in some states, PTs can directly refer a patient for testing (like an ultrasound); in other states, the patient will be referred to a healthcare provider for further evaluation.
PT TAILORED TO THE PATIENT
Dr. Hillegass stresses that there isn’t a “one-size-fits-all” approach to help patients recover and become more mobile. Patients are evaluated individually on what they can physically do and what their goals are so that a successful plan can be developed. “If a patient is not able to stand up, then we do sit-to-stand type of exercises. If the patient has balance issues, we are going to look at balance,” says Dr. Hillegass. The same individualized approach is taken for people with different types of blood clots: if the patient had a pulmonary embolism (PE), or blood clot in the lungs, a cardiopulmonary PT might concentrate first on breathing exercises to improve ventilation and then assess mobility, particularly focusing on the oxygen in their blood and shortness of breath. For a blood clot in a patient’s arm, a PT might work on moving that arm but add compression (using a compression sleeve) to ease any pain.
For patients with other long-term illnesses like chronic obstructive pulmonary disease (COPD), pulmonary hypertension (PH), or chronic thromboembolic pulmonary hypertension (CTEPH), cardiopulmonary PTs must also take lower oxygen levels into account as they help patients become more mobile. Patients with these conditions may get short of breath because the amount of oxygen in their blood may drop during exercise; ultimately, some patients may require oxygen during exercise. In other cases, PTs may use breathing exercises to help patients develop their lung capacity and endurance. PTs should always consider a patient’s blood oxygen level when assessing a patient for a blood clot, since shortness of breath or low oxygen levels could be a sign of PE.
PTs also look closely at a patient’s age and home life to develop individualized plans that are safe and effective, which home health nurses can then help implement. “One of the biggest things we do is emphasize strongly to our case managers or social workers that they need to have PT come in right away to assess if an environment is safe,” says Dr. Hillegass. “We will look at how far the bathroom is from the bed, whether the patient needs extra handrails to get in and out of the tub, if a patient is going to trip over oxygen tubing, etc.”
“We assess a patient’s strength and balance, but it’s all these other little thing sat home that you don’t even think of that are very, very important, especially if the patient is taking a blood thinner. A bad fall could lead to a serious bleed, and we want to avoid that.”
Assistive devices—such as walkers or chairs that help push patients up to stand—can also be used to help patients become more mobile at home.
HOW TO ASK FOR PT
Sometimes, it may not be clear whether PT is part of a patient’s recovery plan. Dr. Hillegass says that you should feel comfortable asking for PT to help improve mobility since reduced mobility is a risk factor for future blood clots. The requests can be simple: “I want therapy to walk better, I want therapy so I feel stronger, I need some therapy to be able to dress myself or cook and clean at home,” says Dr. Hillegass. “And then these care teams will say, ‘oh, function!’ That’s PT and occupational therapy. Let’s call them.”
Dr. Hillegass stresses that having PT as part of a care team is important to long-term patient health. “It makes for a shorter length of hospital stay and better care for the patient. Decreased length of stay and improved function are outcomes that have been demonstrated in the scientific literature.”
WILL INSURANCE COVER PHYSICAL THERAPY?
Physical therapy is a benefit covered by both Medicare and other insurance plans, but coverage depends on the patient’s diagnosis. The amount of therapy that’s approved for patients after a medical issue, including a blood clot, may vary depending on the type of insurance. Dr. Hillegass notes that insurance companies usually limit the number of PT visits for reimbursement; some may cover three appointments while others may cover six or more visits. Dr. Hillegass notes that some patients may see the value in PT and decide to pay out-of-pocket for additional sessions so they can continue to reap the benefits of PT and stay mobile.
PT by video conference (or “tele-rehab”) may also be a covered option for patients who have had blood clots. “If the patient doesn’t have a lot of comorbidities [or other health issues], they’ll be a great candidate for tele-rehab,” says Dr. Hillegass. “However, if the patient has diabetes, high blood pressure, or other conditions, they may not want to do tele-rehab first since there may be other issues that need to be addressed.”
Patients who have had a blood clot or have risk factors for blood clots can review available coverage options for PT through their insurance carriers and talk with their healthcare providers about finding cardiopulmonary PTs with experience in blood clot prevention and management.
*Originally published in The Beat – October 2021. Read the full newsletter here.



