Last updated on
Cholesterol and Blood Clots: What’s the Connection?
Most people think of cholesterol as a bad thing but cholesterol itself is not inherently unhealthy. In fact, it’s a necessary building block within the body. Cholesterol is needed to build healthy cell membranes and also serves as the precursor for a variety of hormones.
However, cholesterol levels that are too high can cause health issues. Research has shown that people with high cholesterol are more likely to suffer from blood clots in both the arteries and the veins. (Arteries carry blood away from the heart to other parts of the body. Veins carry blood to the heart from other parts of the body.) Diseases caused by blood clots, including heart attacks and strokes, are among the leading causes of death in the US, so it’s important to understand how cholesterol impacts blood clot risk, and how you can reduce your risk.
TYPES OF CHOLESTEROL
Although cholesterol itself is always the same molecule, we sometimes refer to different “types” of cholesterol. Cholesterol is carried in the blood on different carrier proteins, also known as lipoproteins.
There are two primary types of lipoproteins in the blood:
- Low-density lipoprotein (LDL) carries cholesterol to the body’s tissues. Although cells do need cholesterol, too much of it can deposit in the walls of arteries, leading to reduced blood flow and other health problems.Because of this, LDL is sometimes known as “bad cholesterol.”
- High-density lipoprotein (HDL) carries cholesterol from the tissues back to the liver; the liver then eliminates excess cholesterol from the body. HDL is sometimes known as“good cholesterol.”
People who have higher levels of LDL are at an increased risk for heart attacks and strokes. In general, higher levels of HDL are considered to be protective and decrease the risk of these issues. However, new research has shown that certain types of HDL may also increase risk, and extremely high levels of HDL may not be ideal.
HOW CAN HIGH CHOLESTEROL LEAD TO BLOOD CLOTS?
When cholesterol levels in the blood (especially LDL cholesterol) are too high, excess cholesterol can adhere to the walls of the arteries. This process is known as atherosclerosis. Over time, these cholesterol deposits harden and form plaque. This hardening process occurs due to a buildup of calcium and fibrin. Fibrin is a protein that’s also involved in blood clotting.
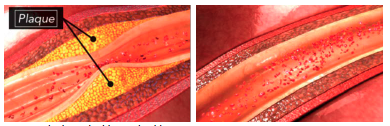
Plaques cause the arteries to narrow and stiffen, leading to a reduction in blood flow. Sometimes a plaque can rupture, meaning that it tears open. Ruptured plaque can trigger the formation of a clot that blocks blood flow through the artery. If this process occurs in the heart or the brain, it leads to a heart attack or stroke.
Research also shows that high LDL levels are associated with a higher risk of clots in the veins. Clots in the veins aren’t triggered by plaques; in fact, plaques only form in arteries, due to the significantly higher blood pressure found there. This means that a different mechanism must be involved when it comes to the risk of venous blood clots, though the exact pathway is unclear.
Some researchers believe that chronic inflammation causes both high LDL and blood clots. LDL cholesterol has also been shown to activate platelets, which can lead to clots. It’s also possible that high LDL doesn’t directly increase blood clot risk, but rather that similar risk factors, such as being overweight, increase both LDL levels and the risk of clots.
HOW TO REDUCE YOUR RISK OF CHOLESTEROL-RELATED BLOOD CLOTS
Controlling your LDL cholesterol levels is important to reduce your risk of blood clots. It’s generally recommended that healthy adults have their cholesterol levels checked at least once every four to six years. You may need your levels checked more often if you have risk factors, such as diabetes or a family history of heart disease.
Make sure that you’re visiting your doctor for preventive care on a regular basis and talk with your healthcare team about how often you should be screened. There are generally no symptoms of high LDL cholesterol, so you’ll need a blood test to find out what your levels are.
Lifestyle changes are always recommended if you have high LDL levels, which include:

CAN CHOLESTEROL MEDICATIONS REDUCE THE RISK OF BLOOD CLOTS?
Your doctor may recommend a cholesterol-lowering medication to reduce your LDL levels. There are a few different options, but statins are the most commonly prescribed medications and research shows that they can reduce the risk of both venous and arterial blood clots.
There are a few possible ways that statins may decrease the risk of blood clots:
- By lowering LDL cholesterol, statins can stop plaques from forming in arteries, which decreases the risk of plaque rupturing and triggering a clot. (However, this effect is only associated with a decrease in arterial blood clots.)
- Statins are believed to influence the expression of certain genes, meaning that they change the levels of certain proteins that cells make. Statins may increase the levels of certain proteins that prevent blood clots.
- Statins are also known to have an anti-inflammatory effect. Because inflammation can lead to blood clots, decreasing inflammation also decreases the risk of clots.
Although statins have been used for decades to lower LDL cholesterol, newer medications, including ezetimibe and PCSK9 inhibitors, are becoming more widely used. These medications have also been found to reduce the risk of blood clots and may have fewer side effects. Some people take both statins and another cholesterol-lowering drug at the same time to get their cholesterol under control.
If you have side effects from your cholesterol medications, talk with your doctor. They may be able to switch your medications or help you manage the side effects so that you can still get the benefits of lowering your LDL.
Remember that even if you’re taking medications, it’s still important to maintain a heart-healthy lifestyle. Keeping your LDL cholesterol under control can help to reduce your risk of serious complications and improve your chances of living a long and healthy life.
*Originally published in The Beat — December 2022. Read the full newsletter here.



