Published on
The Procedure Playbook: A New Educational Resource from NATF
NATF is excited to bring you The Procedure Playbook, our latest resource for people who take medicines to prevent blood clots and need a procedure or operation.
We worked with leading experts to break down complex clinical information into an easy-to-use handbook. You can access the Playbook here.
Why is it important for me learn about clinical guidelines?
The American College of Chest Physicians published updated recommendations on how to make medicine adjustments before, during, and after surgery. These guidelines can help your doctor learn more about the best way to manage your treatment—but it’s also important for you to stay up to date with this information to better understand why and how your treatment might change.
When you are taking medicines to prevent blood clots, even a small procedure requires careful planning. Learning more about clinical guidelines can help you feel better prepared and ready to go.
How will I understand this information? I’m not a doctor!
Since the clinical guidelines are written for doctors, they contain lots of medical jargon and can be difficult to understand. We created this comprehensive, simple guide to help you better understand their recommendations.
Who is this guide for?
This guide is an educational resource for people…
- Who take medicine to prevent blood clots (and have been on the medicine for at least 3 months)
- Who need a planned surgery while on this medicine
This information is not for people who need an emergency operation or a high-risk surgery that could cause a lot of bleeding.
This information is for general educational purposes only—it is not meant to be personalized medical advice. Everyone is different, so it’s important to work with your healthcare team to understand what’s best for you.
What’s in the guide?
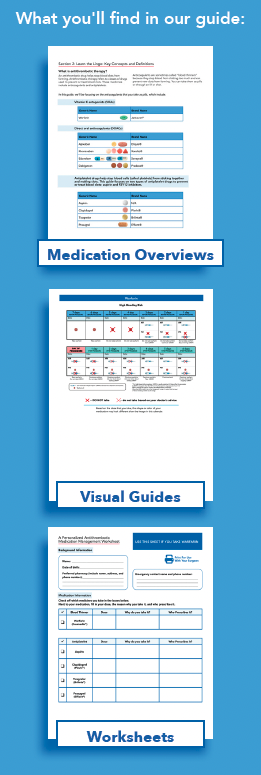
The Playbook includes information from clinical guidelines on how blood clot medicines should be adjusted before, during, and after surgery. These adjustments are different depending on the type(s) of medicine you take and the type of procedure you need.
“The guidebook includes comprehensive information to help patients better understand relevant terminology and their risks of clotting and bleeding around the time of a procedure. It also provides general recommendations about if and when to stop and restart blood thinners or antiplatelet medicines and if and how to use bridging* therapy. It is important for patients to have this information so they can work with their doctor to follow a specific medication plan around the time of their procedure,”
Dr. Spyropoulos
*Bridging is a medical strategy used when patients need to temporarily stop taking warfarin before a medical procedure or surgery.
Perioperative antithrombic management (PAM) planning
Your doctor and healthcare team will create a plan for perioperative antithrombotic management, or PAM. Perioperative means “around the time” of surgery; this can be 1 week before surgery, the day of surgery, or 4 weeks after surgery. This period of time is when the risk of clots or bleeds is highest. The goal of this plan is to make sure that you have a safe surgery by balancing the risk of blood clotting and risk of bleeding.
Each person’s risk of blood clots or bleeding is affected by the type of condition they have, including whether they have a mechanical heart valve. This risk is also affected by the type of procedure. For example, a colonoscopy has a low-to-medium bleeding risk and a bowel surgery has a high bleeding risk. Your healthcare team will take these factors into consideration when creating your PAM plan.
Stopping and restarting your medicines
We know that remembering when to stop and restart your medicines can feel overwhelming, especially with the stress of preparing for a procedure. We’ve included recommendations on how to adjust your specific medicine(s) while considering your risks and the risks of the procedure.
The guide includes personalized medicine management worksheets to help you keep on top of medicine adjustments. You can print these sheets and fill them out with your doctor. These are great resources you can use to discuss when to stop and restart medicines with your healthcare team.
There are also calendars to help you visualize exactly when to make medicine adjustments based on the date of your surgery.
Never stop taking your medications without talking to your doctor first.
*Originally published in The Beat — February 2024. Read the full newsletter here.



