Nov 18 3:00pm
Table of Contents
Program Description
Pulmonary vascular disease (PVD), including pre- and post-capillary pulmonary hypertension, is a spectrum of progressive, symptomatic, and ultimately fatal disorders for which significant advances in treatment have been made. Despite advances in the management of PVD, the mortality rate remains disproportionate. Evaluation and treatment are often delayed until patients present with serious complications. Effective management requires timely recognition, accurate diagnosis, and selection of the different therapeutic options.
Progression to right ventricular dysfunction and finally failure can occur as an acute event in consequences where the pulmonary hypertension develops acutely as with pulmonary embolism, or because of a chronic condition such as pulmonary arterial hypertension, chronic thromboembolic pulmonary hypertension (CTEPH), chronic obstructive pulmonary disease (COPD), interstitial lung disease, or chronic left sided heart or valvular disease.
Early detection and appropriate management can improve quality of life and may improve survival. Medical therapy has come a long way towards decreasing symptoms, enhancing performance, and improving prognosis, but there is still a long way to go, especially for the broader population of patients with PVD.
This program is tailored to clinical and research professionals who study and/or care for patients with right heart disease, congenital heart disease, pulmonary hypertension, and associated disorders.
At the end of this program, participants should be able to:
- Review the options for advanced imaging approaches to assess and monitor RV function and pulmonary vascular remodeling
- Describe pharmacologic interventions to augment or restore RV function in the patient with advanced PVD or critical illness
- Assess the latest interventional, device, and pharmacologic approaches to PVD and evaluate these options in various forms of PVD, including disease-modifying pathways such as PDGF and TGF-beta signaling
- Discuss advanced hemodynamic and physiologic correlates of right ventricular-pulmonary arterial coupling
How to Claim Continuing Education Credit
This program is no longer eligible to claim credit.
Pricing
Earn up to 12.5 CME Credits!
Registration includes:
- Breakfast, lunch, and coffee breaks for both days
- Q&A sessions with experts
- Networking opportunities
| REGULAR RATE | |
|---|---|
| Healthcare Professional (MD/DO) | $300 |
| Allied Health Professional | $225 |
| Fellow/Trainee | $75 |
| Industry | $600 |
| Virtual (Live-stream Only) | $150 |
Refund Policy
NATF will not be reimbursing any event registrations after November 9, 2023. If you’re no longer able to attend the Symposium in person, we will send you a link to attend virtually but will be unable to refund any portion of your registration after the stated deadline.
Speakers
Event Agenda
*Faculty and agenda subject to change
Welcome Remarks
- Assessing the RV: It’s All in the Curves – Francois Haddad, MD
- Assessing the RV: It’s the Dots, Not the Curves: Focus on Speckle Tracking and Strain Imaging – Monica Mukherjee, MD, MPH
- Is There a Role for PET or Molecular Imaging to Assess the RV? – Paul B. Yu, MD, PhD
- Advanced Imaging Approaches to Assessing Pulmonary Vascular Remodeling and RV Function – Farbod N. Rahaghi, MD, PhD
- Panel Discussion
Break
- Vasopressor Support in RH Failure – Can We Optimize RV Mechanics and Coronary Perfusion? – Bradley M. Wertheim, MD
- Inotropic Support in RV Failure – Is There Really a Role? – Hilary M. DuBrock, MD
- When to Consider MCS – Hemodynamic, Physiologic, and Patient Selection – Manreet K. Kanwar, MD
- When and why is the RV too Sick for Lung Transplantation? – Nirmal S. Sharma, MD
- Panel discussion
Lunch Break
Assessing Right Ventricular Function Using Exercise, Imaging, and Hemodynamics – Anton Vonk Noordegraaf, MD, PhD
Break
- RV-PA Coupling, Afterload, and Pressure-Volume Curves – Paul Heerdt, MD, PhD
- Pulmonary Artery Hemodynamics: the Action is in the Proximal Vasculature – Franz Rischard, DO, MSc
- Pulmonary Artery Hemodynamics: the Action is in the Small Vessels – Inderjit Singh, MD, FRCP
- Clinical Implications of Aggressive Afterload Reduction – Eileen M. Harder, MD
- Panel discussion
Welcome Remarks and Announcements
- Clot In Transit – What is the Optimal Approach? – Gregory Piazza, MD, MS
- What does Clot Burden Mean? – Josanna Rodriguez-Lopez, MD
- Provoked and Unprovoked – What is the Difference, and does it Matter? – Behnood Bikdeli, MD, MS
- Optimal Duration of Anticoagulation – 2 months; 3 months; life long? – Alison Witkin, MD
- Panel discussion
Break
- Intrapulmonary Artery Balloon Pump – Why and When? – Jane A. Leopold, MD
- Targeting BMPR2 – Marius Hoeper, MD
- Targeting Metabolism – is it a Viable Target? – Sebastien Bonnet, PhD
- In the Age of Disease Modifiers, What Should our Approach to Treatment be? – Roham T. Zamanian, MD
- Panel discussion
Lunch Break
- Pulmonary AVM’s without HHT – Alexandra K. Wong, MD
- Anomalous Venous Return – Diagnosis and Management – Ada Stefanescu Schmidt, MD, MsC
- Left to Right Shunting and Enhanced Pulmonary Blood Flow – Why is the Patient Dyspneic? – Phillip Joseph, MD
- Pulmonary Artery Aneurysm – is it a Surgical Disease? – Harrison Farber, MD
- Panel discussion
Closing Remarks
Sponsorship Information
If you are interested in sponsoring the Right Heart Symposium, please contact Kathryn Mikkelsen at [email protected]
GOLD SPONSORS
United Therapeutics Corporation
SILVER SPONSORS
Janssen Pharmaceuticals
Merck
Pharmosa Biopharm Inc.
START-UP SPONSORS
Aria CV
AI Therapeutics
Liquidia
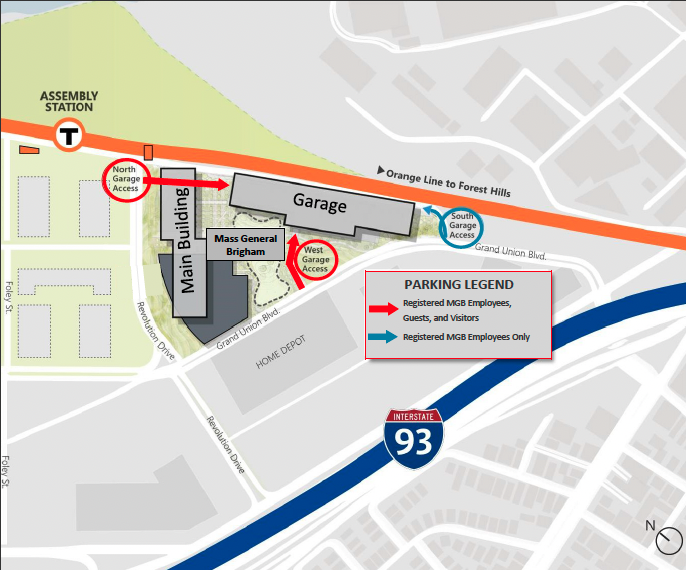
Event Location
Mass General Brigham Assembly Row
399 Revolution Drive
Somerville, MA 02145
Markell Room ABC
Click here for detailed directions
Accreditation

In support of improving patient care, this activity has been planned and implemented by Boston University Chobanian & Avedisian School of Medicine and North American Thrombosis Forum. Boston University Chobanian & Avedisian School of Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Boston University Chobanian & Avedisian School of Medicine designates this live activity for a maximum of 12.5 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Contact Hours: 12.75

Boston University Chobanian & Avedisian School of Medicine has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 12.5 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation
Planning Committee
- Aaron B. Waxman, MD, PhD
- Jane Leopold, MD
- Alexandra Wong, MD
- Bradley Wertheim, MD
- Charlie Lee, PA-C
- Deborah Whalen, APRN, MSN
- Eileen Harder, MD
- Farbod Rahaghi, MD, PhD
- Stephanie Perella, PA-C