Last updated on
Falls and Anticoagulation: What You Should Know
Table of Contents
KEY POINTS
- Blood thinners, or anticoagulants, help prevent blood clots but can increase the risk of bleeding.
- Falling is a major reason why some people hesitate to take blood thinners.
- Falling is a common risk as people age, but other factors that can increase the risk is poor lighting, slippery floors, and vision issues.
- Talk to your doctor to weigh the risks and benefits of taking anticoagulants.
- Exercise can help prevent falls by strengthening muscles.
- Review medications with your doctor or pharmacist to avoid potential fall risks.
- If you fall while on a blood thinner, contact your healthcare provider right away.
- To prevent future falls, you can make your homes safer, wear proper shoes, stay active, and keep track of their medications.
FULL SUMMARY
Anticoagulants, also known as blood thinners, are effective in treating and preventing blood clots, but they increase the risk of bleeding. The fear of falling—and subsequently bleeding from a fall—is a major reason why some patients hesitate to take blood thinners. Healthcare providers also cite fall risk as the most common reason for not prescribing anticoagulation. “Anyone on anticoagulation is going to bleed easier, so if you’re taking anticoagulation and you fall or injure yourself, you’ll bleed more easily than someone who isn’t on anticoagulation,” explains Dr. Judith Beizer, a clinical professor at St. John’s University College of Pharmacy and Health Sciences in New York. “Bleeding isn’t always visible. You could bleed internally and not know it, and that’s a significant concern. For example, we worry about brain bleeds when people fall and hit their heads – but if patients don’t see blood, they might not realize that they’re bleeding,” she says.
The risk of falling increases as patients age and become less mobile, but there are other common risk factors that patients and caregivers may overlook.
- Environmental factors: Electrical cords, slippery floors, loose carpets/rugs, poor lighting, and stairs all pose a risk for falling at home.
- Vision issues: Vision declines with age and poor vision can lead to falls – but vision correction is also a culprit for falling. Bifocal glasses, for example, can make things blurry if they’re worn while walking down a flight of stairs.
- Shoes: Ill-fitting shoes can raise the risk of a fall.
- Medications: Medicines that cause dizziness, drowsiness, blurred vision, or problems with coordination increase fall risk. People on diabetes medications can also be at risk for falls if their blood sugar is either too tightly controlled or too low.
Does the type of anticoagulant matter when it comes to fall risk? According to Dr. Beizer, “the anticoagulant itself doesn’t affect your risk of falling. Based on what we know, your risk is your risk whether you’re on warfarin or a direct oral anticoagulant (DOAC). We’re more concerned with weighing the risk of bleeding and the risk of falling against the risk of not being anticoagulated.”
In patients with atrial fibrillation, for example, anticoagulation can significantly lower the risk of having a stroke. “In my experience, patients fear a stroke more than a fall or a bleed. So, in most cases, I think it’s important for those patients to be on a blood thinner. But with decisions like this, you need to understand your level of risk and the doctor needs to document that risk. The decision to start a blood thinner should only be made after you have a conversation with your doctor. For patients who start anticoagulation but worry about falling, it’s again important to address those risk factors that are within their control, like making sure that the home is well-lit, that they get their eyesight checked, etc.”
Exercise is also important for staving off falls. “It’s a common misconception that a person should avoid exercising to avoid a fall. Exercising can actually help strengthen the bones and muscles needed to prevent a fall,” Dr. Beizer explains. “I like to say that if you don’t use it, you lose it, and those weakened muscles can lead to falls.”
In addition, Dr. Beizer encourages a formal medication audit at least once a year. She recommends bringing all medications to your primary care doctor or to a pharmacist and reviewing the dosage and instructions for each prescription. “This review is especially key for patients who are on many medications. These patients often have different providers prescribing meds for different issues and it’s important to keep the medication list up-to-date. Patients who take certain anticoagulants also need to take them at the exact same time every day, so it’s helpful to go over the protocols more than once with a doctor or pharmacist.”
Patients who work with an anticoagulation management service (or a “coumadin clinic”) can consult the pharmacists there about their medications. Patients who don’t visit a clinic can consult a pharmacist at their local pharmacy. “Many patients don’t realize that they can ask their local pharmacist. The pharmacists there are an easily available resource for you,” says Dr. Beizer. The American Society of Consultant Pharmacists (ASCP) or Board of Pharmacy Specialties (BPS) can also help connect you to a local pharmacist.
So, what should you do if you have a fall while on a blood thinner? Dr. Beizer recommends calling your healthcare provider as soon as possible. “You should be assessed for bruising, and most importantly, for potential head trauma. Your doctor will want to know how you fell, what parts of your body were affected, and if you lost consciousness. Even if you think the fall was minor, you should still call your doctor.”
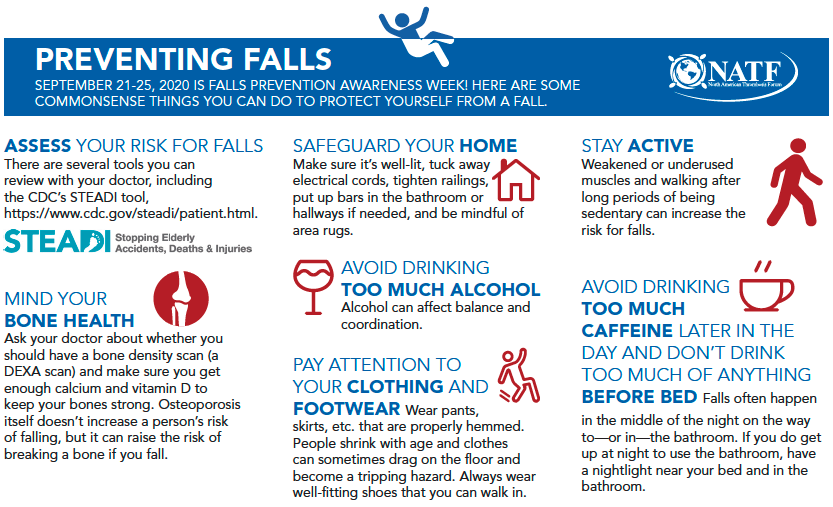
There are several things patients can do to prevent future falls as well. [See below]. “Most importantly, try to make your home as “fall-proof” as possible, wear shoes that t well, stay active, keep tabs on your medications, and know that your pharmacist is your friend and can help you manage your anticoagulation and fall risk!”

*Originally published in The Beat – August 2020. Read the full newsletter here.



