Last updated on
The First Six Months
A look at life after a blood clot
THE BODY’S RESPONSE
Once you’ve had a blood clot, your body might break it down and absorb it, depending on its size and location. In other cases, your body might not absorb the clot(s) but can still function without any problems. If you have questions about how your body is responding to your blood clot, your doctor or healthcare team can provide more personalized information.
ANTICOAGULATION
After being discharged from the hospital, you may be put on an anticoagulant for six months or more.
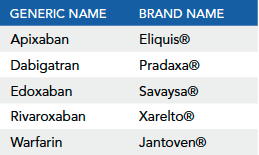
Anticoagulants are medications that are used to stop blood clots from getting larger. These drugs are sometimes called “blood thinners,” although they don’t actually thin the blood. They also can’t dissolve existing clots but can prevent new ones from forming. Anticoagulants are typically prescribed for the first 3-6 months after a deep vein thrombosis (DVT) or pulmonary embolism (PE). However, research shows that thrombosis (blood clots) may be a chronic disease. According to Dr. Samuel Goldhaber, the Director of Brigham and Women’s Hospital’s Thrombosis Research Group and President of the North American Thrombosis Forum (NATF), people who’ve had a DVT or PE have a higher risk of developinganother blood clot. For this reason, some patients may require more than 6 months of anticoagulation. Talk to your doctor about how long you’ll need to take a blood thinner and if you’ll require extended therapy. There are several anticoagulants available to treat and prevent blood clots:
Warfarin
Warfarin is a vitamin K antagonist (VKA). VKAs work by blocking vitamin-K-dependent clotting factors in the blood. Warfarin has been used for decades to treat blood clots, but it comes with some challenges.
INR LEVELS
Patients on warfarin need to visit a clinic regularly to have their international normalized ratio (INR) levels tested. An INR level measures how much time it takes for your blood to clot. Most patients need to maintain an INR level between 2 and 3 to be considered in “therapeutic” (or target) range. An INR below the therapeutic range increases the risk of clotting while an INR above 3 increases the risk of bleeding.
MANAGING INR LEVELS
INR levels can change from day to day and many patients struggle to maintain a consistent level, despite their best efforts. Studies show that at any given time, only about 60% of patients have INR levels within target range.
Several lifestyle factors can affect INR levels, including diet. Remember that warfarin reduces the action of vitamin K in the body (to prevent blood clots), so eating foods high in vitamin K can make warfarin less effective. Some of these foods include kale, spinach, broccoli, and Brussels sprouts. You can still eat these foods if you take warfarin, but you should eat a similar portion consistently; that way, your warfarin dose can be adjusted to account for the extra vitamin K you’re getting from these foods.
You should also be cautious about drinking alcohol while on warfarin. Guidelines recommend avoiding alcohol entirely, but if you do consume alcohol, you shouldn’t drink more than 1-2 drinks a day. Alcohol can be a problem if it changes how the body metabolizes warfarin.
INR MONITORING
Point-of-care INR testing refers to testing done in a lab or a clinic. The testing itself involves a fingerstick to draw blood. The blood sample is put onto a test strip and placed in a coagulometer, which is a device that analyzes the sample and provides an INR reading.
For some patients, the need to routinely visit a clinic for INR testing can be inconvenient. Depending on your insurance coverage, home testing may be a better option. Home testing requires a kit that includes an INR monitor and testing strips similar to those used in clinics. A medical professional can teach you how to use the machine and self report your INR levels to your clinic.
Whether you test in a lab or at home, an anticoagulation management clinic can help you keep your INR levels in the target range. Ask your doctor if there’s an anticoagulation management service available in your area. For more information on home INR testing, please click here.
Direct oral anticoagulants (DOACs)
Although warfarin has dominated the market for decades, DOACs are now the recommended, guideline-approved treatment for thrombosis. These drugs include apixaban, dabigatran, edoxaban, and rivaroxaban.
DOACs have several advantages over warfarin. “In general, the DOACs are more effective and they’re safer, particularly with respect to serious bleeding. DOACs cause half as much fatal bleeding than warfarin. They’re also more convenient – they don’t require routine blood monitoring and can be given safely in fixed doses,” explains Dr. Christian Ruff, Director of General Cardiology at Brigham and Women’s Hospital.
However, one key concern with DOACs has been their reversibility; reversal agents for these drugs weren’t available until recently. There are now two FDA-approved reversal agents: idarucizumab and andexanet alfa.
Idarucizumab, approved in 2015, reverses dabigatran. It’s often used in cases where a patient needs emergency surgery or has a life-threatening bleed.
For apixaban and rivaroxaban, a reversal agent called andexanet alfa “appears to work well and is safe,” says Dr. Ruff. “It acts as a decoy that binds to the clotting factors at play and prevents them from exerting their anticoagulant effects.” The FDA approved andexanet alfa in 2018.
When it comes to medication, every patient can have a different experience based on their medical and family history, their diagnosis, their lifestyle, and more. Always consult your healthcare provider if you have a question about your medications. Pharmacists are also a valuable resource and can answer questions about medication dosages, side effects, and interactions.To learn more about DOACs vs. warfarin, click here or download our Anticoagulant Comparison Chart.
Follow-up care
After a blood clot, you should follow up with your primary care provider and establish a network of care. You may also be referred to a specialist, such as a cardiologist, hematologist, pulmonologist, or vascular medicine specialist. These specialists can help steer you towards the best treatment for your individual needs.
Follow-up is especially important if you’ve had an inferior vena cava (IVC) filter put in your body. An IVC filter is a device to stop clots from traveling from the legs to the lungs. These filters are often temporary and will be removed afterthe risk for PE or DVT has gone down.
After a clot, you may believe that an ultrasound should be part of your follow-up care to see if your clot has gone away. However, an ultrasound is only necessary if you’re experiencing new or worsening symptoms or if you’re changing medications. Many patients also retain some residual clot—much like a scar—that’s absorbed into the wall of the vein and can be seen on ultrasound. These “scars” aren’t necessarily associated with a poor outcome.
GENETIC TESTING
There are some genetic mutations that can make you or your family members more likely to get blood clots. The two most common mutations are Factor V Leiden and the prothrombin gene mutation.
Genetic testing is a personal decision. Using genetic testing to screen for blood clots is not currently recommended. If you’d like to learn more about testing, please visit the National Human Genome Research Institute website and talk to your doctor.
Complications after a blood clot
It’s important to pay attention to what your body is telling you.
If you’ve already had a blood clot, you have a higher risk of having another clot compared to the general public. (Patients who’ve experienced a blood clot are roughly 25% more likely to have a second episode.) This risk goes down the longer that it has been since your clot and varies from person to person – but it’s still important to watch out for the warning signs of a new blood clot, especially as the risk of developing a clot increases as you age.
Remember that DVT symptoms include swelling and pain in the legs, especially behind the knee. The pain often feels like a long-lasting cramp. PE symptoms often appear in the chest or in the back and include pain, shortness of breath, fatigue, or coughing up blood.
After a DVT or PE, it’s normal to experience some discomfort as you recover.
After a DVT, you may still have swelling and soreness in your legs, called post-thrombotic syndrome. Likewise, you could experience mild chest pain, back pain, or shortness of breath after a PE. Patients with PE are also at risk for developing a condition called chronic thromboembolic pulmonary hypertension (CTEPH). CTEPH occurs when a blood clot in the lungs causes high blood pressure in the lung vessels. Again, recovery after a blood clot can be different from patient to patient. It can also be difficult to distinguish between the symptoms of a new blood clot and the pain from a previous one. Always contact your doctor if you have concerns about new or ongoing symptoms.
COMPRESSION STOCKINGS
Compression stockings can help you manage uncomfortable swelling after a DVT and can prevent additional problems.
Many doctors prescribe compression stockings to treat ongoing swelling and pain after a DVT or to help patients manage post-thrombotic syndrome. Some stockings apply the same amount of pressure to a covered area, while others apply different amounts of pressure to parts of the leg. Stockings come in knee-high or thigh-high lengths, but the length and pressure are personalized to each patient. Always use the compression stockings that are prescribed for you. Over-the-counter compression stockings are less effective.
Dr. Goldhaber recommends that patients wear the stockings for two years after a blood clot. It’s important to replace compression stockings every 3 months since the compression breaks down over time.
ACTIVITIES
Stay active but be mindful.
One of the most common lifestyle questions that patients have after starting anticoagulation is “when can I resume my normal activities?” Dr. Goldhaber recommends that patients on blood thinners avoid vigorous activities such as skiing, boxing, playing football, horseback riding, etc. These activities could cause falls, concussions, or other injuries and result in serious bleeding in an anticoagulated patient.
However, avoiding contact sports/activities does not mean that you should avoid exercise altogether. In fact, exercising after a blood clot is a major part of recovery. Physical activity not only improves heart health, but also helps prevent recurrent PE or DVT.
“If you’ve recently had a PE, you may feel short of breath, have chest pain, and/or become easily fatigued when you start exercising. After a DVT, your leg may be swollen, tender, red, or hot to the touch,” explained Dr. Stephanie Lew, a Boston-based physical therapist. “These symptoms should improve over time, and exercise often helps. Walking and low-impact exercise are safe but be sure to listen to your body to avoid overexertion.”
If you have an activity that you’d like to get back to or if you want to start exercising, be sure to consult your doctor beforehand.



