Last updated on
Food for Thought: Vitamins, Diet, and Anticoagulation
Tara Lech, PharmD is an Anticoagulation and Cardiovascular Clinical Pharmacy Specialist and currently serves as the Thrombosis Program Manager at Lahey Hospital and Medical Center in Burlington, MA. She recently joined NATF for an interactive Ask the Expert panel and answered several questions about anticoagulation, vitamins, supplements, herbs, and food. If you take a blood thinner, here’s what you should know.
Q: What can you tell us about interactions between anticoagulants and vitamins or nutritional supplements?
It’s challenging to navigate the world of supplements, and that’s why it’s so important to make your anticoagulation provider aware of any supplements that you’re taking. Even though supplements are available over the counter (OTC), it doesn’t mean that they’re risk-free. Some very common supplements and herbs can have a significant anticoagulation effect and may impact your body’s ability to either clot or bleed. Another thing to keep in mind is that supplements are not regulated, so there may be differences in manufacturing that could affect risk as well.
Q: Which herbs or supplements most commonly interact with anticoagulation?
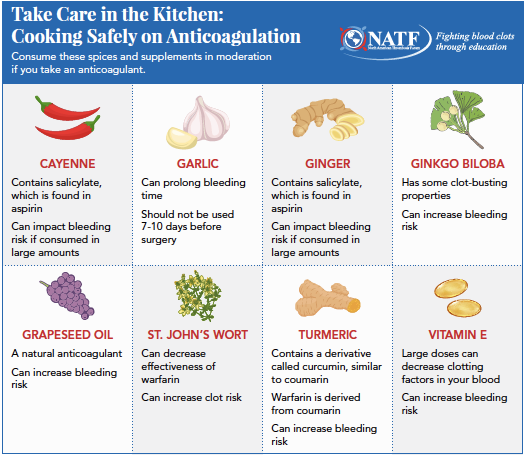
Some of the big ones that we see in my clinic are herbs, like turmeric, ginger, or garlic, and oils, like grapeseed oil, as well as some OTC supplements, such as ginkgo biloba and vitamin E. There are several things to consider before using these herbs or supplements.
Q: Since many herbs and spices are commonly found in foods or used in cooking, what should people be aware of if they’re on anticoagulation?
Food interactions are more of a concern with warfarin than with direct oral anticoagulants (DOACs), and I always tell my patients to remember that taking warfarin isn’t a “life sentence.” While there can be some interaction between warfarin and the vitamin K in food, you can still eat what you want in moderation. It’s important to know that you don’t have to eat the same exact things every day, you don’t have to count how much vitamin K is in every food you eat, and you can enjoy your favorite herbs and spices. I wouldn’t recommend eating 10 cloves of garlic every night – but you probably wouldn’t want to do that anyway!
The same thing goes with alcohol. We are not saying that you can never have a drink because you’re on a blood thinner – we just recommend drinking in moderation. If you know you’re going to be drinking a little more than normal—around the holidays, for example—then you might not want to schedule your INR* test for the next day because you need to give your body time to level out. However, I do caution patients that if you take warfarin and have more than two drinks a night, you’re increasing your risk of bleeding. So again, I can’t stress enough that moderation is key, and your care team is always happy to connect you with resources if you need help cutting back.
*INR = international normalized ratio, a level that measures how much time it takes for your blood to clot. Most patients need to maintain an INR level between 2 and 3 to be considered in “therapeutic” (or target) range. An INR below the therapeutic range increases the risk of clotting, while an INR above 3 increases the risk of bleeding. INR levels are only monitored in patients who take warfarin and are not useful in patients who take DOACs.
Q: With cold and flu season and, of course, the COVID-19 pandemic, vitamins C and D have been in the news. What can you tell us about using these vitamins when taking anticoagulation?
If you’re taking supplemental doses of vitamin C or D, we wouldn’t ask you to stop that – we would just note it in your patient record and see how you respond. During cold and flu season, many patients take vitamins C and D in hopes of boosting their immune system and improving their overall health. There is no evidence that these vitamins will lessen your risk of getting either the flu or COVID-19, but we do know they’re essential to a healthy immune system, along with rest, hydration, and proper nutrition. It’s important to let us know what immune boosters and vitamins you’re taking, so that we can make sure they don’t interact with your anticoagulation, or with one another.
Q: Finally, laws are changing across the country and people have more access to cannabis and CBD than ever before. Is there any evidence that these products affect anticoagulation?
First, I think that we really need to destigmatize talking about cannabis and CBD, precisely because of the increased access to these products. You shouldn’t be afraid to tell your provider if you’re regularly using marijuana or CBD oils, tablets, or other edible products. In fact, you really need to be telling us because there is evidence that cannabis and CBD can interact with certain medications, including blood thinners.
For starters, cannabis has the potential to:
-
- Inhibit platelet production, leading to an increased risk of bleeding
- Decrease the effects of antiplatelet medications by slowing down the metabolism and increasing the risk for a cardiac event
- Increase the effects of warfarin, resulting in a higher INR and an increased risk of bleeding
- Increase the effects of DOACs by slowing down the metabolism of the medication and increasing your risk for bleeding
Remember that as providers, we’re here to help you. Shared decision-making is very important in the anticoagulation world, but for us to make decisions with you, we need to know what you’re using in combination with your anticoagulation. We want to tailor care, make sure that you’re safe, and help you achieve all of your healthcare goals.
*Originally published in The Beat – December 2020. Read the full newsletter here.



