Last updated on
KEY TAKEWAYS
- The chance of getting a blood clot from traveling is small but some people have a higher risk, like those who are overweight, older, or pregnant.
- To lower the risk of getting a clot when traveling by plane, experts recommend moving around every 1-2 hours and drinking lots of water.
- People at higher risk may need to wear compression stockings or talk to their doctor about taking medicine to prevent blood clots.

Dr. Susan Kahn
Long-distance travel may raise your stress level, but can it also raise your risk of getting a blood clot?
To learn more, we spoke to Dr. Susan Kahn, a Professor of Medicine at McGill University and a Canada Research Chair in venous thromboembolism (VTE).
HOW DOES PLANE TRAVEL INCREASE MY RISK OF A BLOOD CLOT?

Blood clots affect about 1-2 in 1,000 Americans per year, and the risk may double or triple after a flight that’s 4+ hours. Some studies estimate that 1 in 4,600 travelers will have a blood clot within 4 weeks of a long flight.
According to Dr. Kahn, “the risk of a travel-related blood clot is quite small, and the average traveler doesn’t need to worry about it. Billions of people travel by plane every year, and most of them don’t get a blood clot.”
However, those who already have risk factors for a clot may have a higher risk of developing travel-related VTE. These risk factors include:
- Obesity
- Age over 40
- Use of birth control pills or hormone therapy
- Recent injury or surgery (within last 3 months)
- Limited mobility
- Pregnancy and up to 3 months after birth
- A personal or family history of blood clots
- Active cancer or recent cancer treatment
It’s unclear if long-distance air travel is any riskier than car or train travel, but there are factors unique to airplanes that can affect risk:
- Air travelers sit in a tight space with the back of the knee pressed against the seat. The vein behind the knee is a common area for clots to form.
- Immobility can raise the risk of a clot. Your seat assignment, turbulence, and other factors can make it difficult to move around easily.
- Your body takes in less oxygen when the air pressure low. Some data suggest that lower oxygen levels can trigger the body’s clotting response.
- Dehydration can also increase the risk of a clot. Drinking coffee or alcohol on a flight can fast-track dehydration.
- Many people sleep on flights – and if you’re sleeping, you aren’t moving or hydrating.
HOW CAN I REDUCE MY RISK OF GETTING A CLOT?
The good news is that there are several commonsense methods recommended by clinical guidelines that can help lower your risk:
- Choose a bulkhead seat, try booking an aisle seat, or ask if your flight offers extra-legroom seating.
- Try to move around the plane every 1-2 hours.
- Avoid sleeping in awkward positions for long periods of time.
- Try not to cross your legs.
- Avoid wearing tight clothing.
- Drink lots of water and avoid alcohol, caffeine, and sedatives.
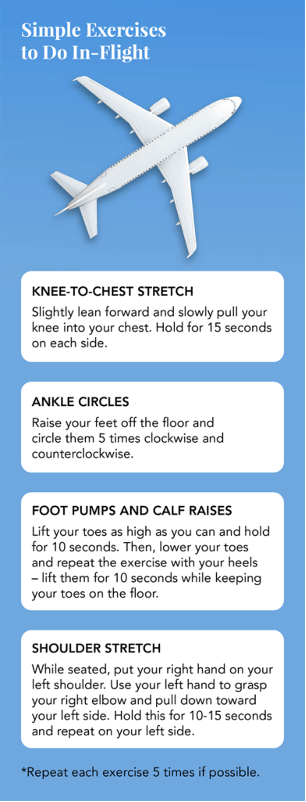
- Do some simple exercises in your seat to improve blood flow.
“For the average healthy person taking a long flight, we don’t recommend anything other than commonsense measures, like walking around the plane and staying hydrated,” explains Dr. Kahn.
Since there’s still a limited amount of data on travel-related VTE, the right course of action may be different for each person.
THE BOTTOM LINE
Travel-related blood clots are rare BUT moving around and staying hydrated are two ways to stay healthy – both in flight and on the ground. Talk to your doctor if you’re concerned about developing a blood clot while traveling.
Learn more about the risks of getting a blood clot here.
REFERENCES
Study of Blood Clots in a Racially Diverse Population Finds Differences in the Rate of New Cases and Deaths by Race – Centers for Disease Control and Prevention
Travel-associated Venous Thromboembolism – Wilderness & Environmental Medicine
Blood Clots and Travel: What You Need to Know – Centers for Disease Control and Prevention
Deep Vein Thrombosis – StatPearls
Hypoxia Induces a Prothrombotic State Independently of the Physical Activity –
PLoS One
Travel-related Venous Thromboembolism – Vascular Medicine
Deep Vein Thrombosis & Pulmonary Embolism – Centers for Disease Control and Prevention
Exercises for Air Travel – Cleveland Clinic Journal of Medicine



