Published on
Understanding Peripheral Artery Disease
Peripheral artery disease (PAD) is a condition that’s unknown to many, yet it affects more than 230 million people worldwide. In the U.S. alone, it’s estimated that more than 8.5 million people live with PAD, putting them at risk for serious complications. Here’s what you need to know about this seemingly silent disease.
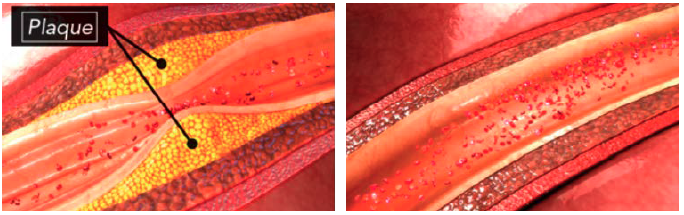
DEFINING PAD

PAD is characterized by a narrowing of the arteries that carry blood from the heart to other parts of the body. This narrowing, medically known as stenosis, ultimately impairs blood flow. “Most PAD cases are related to atherosclerosis—plaque buildup—which causes blockages in the arteries,” says Dr. Jennifer Ballard-Hernandez, a Cardiology Nurse Practitioner, Assistant Clinical Professor at the University of California, Irvine, School of Nursing, and NATF Medical Advisory Board member. PAD most commonly affects the lower half of the body (called lower-extremity PAD), and occurs when plaques build up in artery walls, narrow the walls, and reduce the flow of blood to the legs and feet.
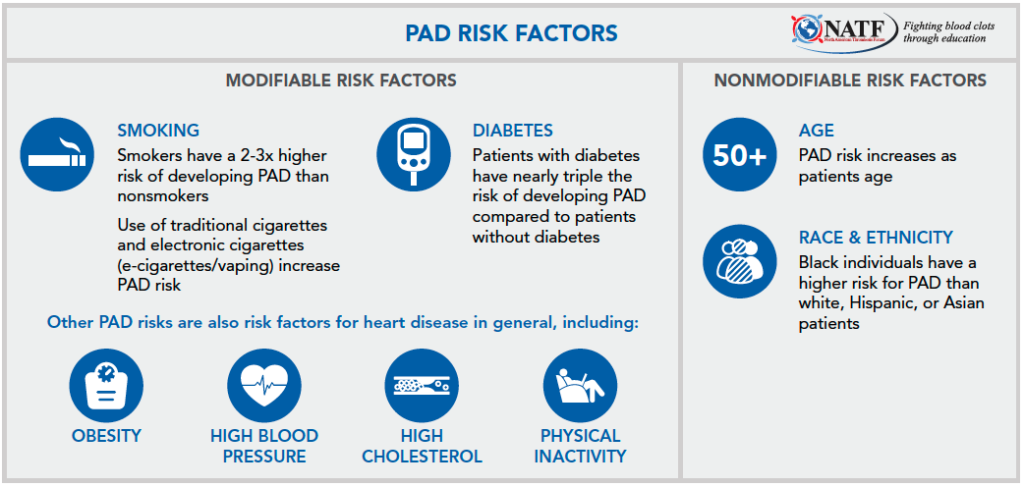
RISK FACTORS
“As with other conditions, we look at PAD risk in terms of modifiable factors—things we can change—versus nonmodifiable risks, which are ultimately out of our control,” Dr. Ballard-Hernandez explains.
SIGNS AND SYMPTOMS

One of the classic signs of PAD is intermittent claudication, which refers to cramping, pain, or weakness in the legs brought on by exertion and relieved by resting. This pain can sometimes be felt all the way down the leg, affecting the buttocks, thighs, and calves. “We often find that intermittent claudication occurs in around 10 minutes. My patients will tell me that after only minutes into their walk around the block, they have to stop because of pain in their leg, which goes away once they stop walking,” Dr. Ballard-Hernandez explains. “The quick onset of pain along with pain relief at rest are two of the key things that differentiate PAD-related pain from muscle soreness, bone/joint pain, or a blood clot in the leg. Musculoskeletal pain doesn’t come on so quickly into exercising and rest may not entirely relieve it. And with a blood clot, there’s usually more swelling or redness in the leg.”
Importantly, not all patients with PAD will experience symptoms, which is one of the reasons that the condition is both underappreciated and underdiagnosed. “Many patients try to go about their daily lives and sometimes don’t recognize that they used to be able to walk 2 miles and now struggle with walking a block. They don’t always appreciate that change in their functional status and instead try to adapt to it, which ultimately can delay diagnosis.”
PAD caused by atherosclerosis is associated with a higher risk of complications, including limb ischemia and stroke. Acute limb ischemia (ALI) is a sudden episode of hypoperfusion—severely diminished blood flow to the limb—and generally occurs over a period of less than 2 weeks. Critical limb ischemia (CLI) is a severe manifestation of PAD marked by chronic pain at rest, ulcers, wounds, or gangrene in one or both legs. The most devastating consequence of CLI is amputation of the affected limb.
WHEN TO SEE A HEALTHCARE PROVIDER

According to Dr. Ballard-Hernandez, leg pain that resolves at rest typically doesn’t warrant an emergency room visit – but it should be addressed as soon as possible at an outpatient appointment with either a primary care provider or cardiologist. Even if you don’t have PAD symptoms, you may need to be screened if you’re older than 65 or over the age of 50 with a history of diabetes, high blood pressure, high cholesterol, or smoking.
However, if you experience any symptoms of limb ischemia, you should be evaluated right away in the emergency room. These symptoms include:
- Sudden, severe limb pain with a change in color (pallor)
- A lost or absent pulse in the foot with numbness and/or tingling
- A change in temperature where the foot becomes cold
DIAGNOSIS
The first step in diagnosis is a screening history, which can be done in any healthcare setting with any type of provider and will include questions about your risk factors and any history of claudication. For the patient without symptoms, “it’s all about risk factor review and modification,” says Dr. Ballard-Hernandez. “If I have patient who comes into my clinic, and they have high cholesterol, high blood pressure, a history of a heart attack or stroke, or if they smoke, that’s someone that I will definitely be screening for PAD.”
After that, diagnostic steps may include:
- Physical exam: Certain signs of PAD can be identified on exam, such as changes in pulses near obstructed arteries, evidence of restricted blood flow, and open ulcers or wounds.
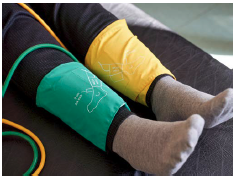
- Ankle-brachial index (ABI): After the screening questionnaire and physical exam, the ABI is the first-line test done to diagnose PAD. A blood pressure cuff with a Doppler probe is used to get a blood pressure reading in the ankle. That number is then compared to the blood pressure measurement from your arm. Most primary care offices can perform ABI tests.
Additional diagnostic tests may include ultrasound and angiography. Angiography is a procedure that uses injectable dye to see how your blood flows through your arteries. Angiography is somewhat invasive and typically used when providers suspect severely compromised blood flow.
TREATMENT
The overall goals of PAD treatment are to manage symptoms and reduce the risk of heart attack, stroke, and amputation.

Lifestyle changes are a key first step. According to Dr. Ballard-Hernandez, “if you smoke cigarettes or e-cigarettes, quitting is the most important thing you can do to prevent PAD-related complications. If you have high cholesterol or diabetes, eating a healthy diet and controlling your blood sugar is pivotal. I’m also a big fan of structured exercise programs, which are typically offered in physical therapy or cardiac/pulmonary rehab settings. These programs are recommended by our cardiology guidelines and will ultimately help you improve your exercise tolerance and quality of life.”
There are also several medication options available. Cholesterol-lowering drugs (statins) are recommended for all patients with PAD. You may also be a candidate for blood pressure medication to control hypertension or medication to help control blood sugar if you have diabetes. Select patients may also be candidates for medications like aspirin or clopidogrel (antiplatelet agents) or rivaroxaban (a blood thinner). These medicines can reduce major heart and limb events. Dr. Ballard-Hernandez recommends talking with your provider to determine what therapies are appropriate for your specific condition.

If lifestyle changes and medications don’t treat PAD entirely, you may be a candidate for revascularization, which is a procedure done by a vascular specialist to help restore blood flow.
If there’s one thing Dr. Ballard-Hernandez wants patients to know, it’s this: “PAD is not a death sentence. We have good screening tools to identify PAD, and a variety of therapies to reduce heart and limb events and prevent the progression of PAD. With tailored medical therapy and structured exercise, we can improve your symptoms and quality of life while lowering your cardiovascular risk.”
REFERENCES
American Heart Association. Peripheral Artery Disease. Updated June 2021. Accessed July 2021.
Berger JS, Newman JD. Overview of peripheral artery disease in patients with diabetes mellitus. UptoDate. Updated June 2021. Accessed July 2021.
*Originally published in The Beat – August 2021. Read the full newsletter here.



