Last updated on
Is Telehealth the Future of Healthcare?

Telehealth has become an important tool for patients and providers during the COVID-19 pandemic. However, there are still many questions about whether it’s the right fit for all patients, since it can pose challenges and barriers for patients of different ages and backgrounds.
To help us look more deeply at telehealth services, we spoke with Dr. Lauren Eberly is a cardiovascular fellow at the University of Pennsylvania. Her work focuses on identifying issues related to inequity in healthcare and developing strategies to make healthcare services more accessible in the US and around the world.
Q: Tell us about your research related to telehealth services.
When we had to abruptly transition to seeing patients using telephone or video conferencing because of COVID-19, we were worried about patients that we might be leaving behind or potentially not reaching with telehealth services.
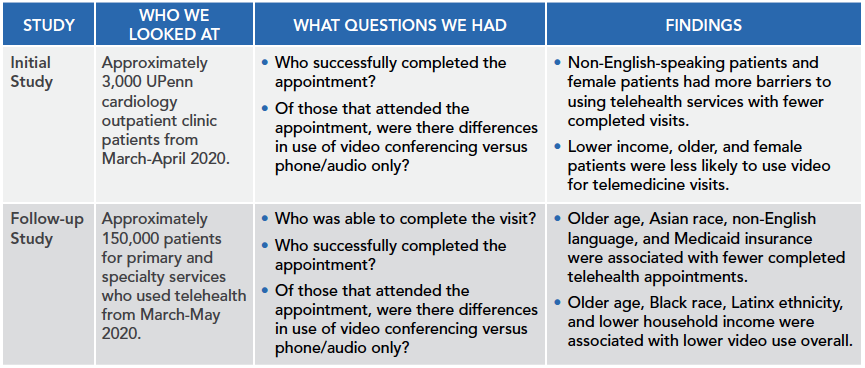
To help answer these questions, we did two studies.
Q: Were you surprised by the findings?
In some cases, yes. For example, it was interesting that Black and Latinx patients completed more primary care and specialty visits but had lower video use as part of telehealth visits. This finding indicates that telehealth has the potential to increase access to care and can be leveraged to reduce disparities, but that some barriers remain that we need to address. We must be intentional with implementation to ensure that all patients are equipped to effectively participate in telemedicine. We also discovered that female patients were less likely to use video conferencing. There could be lots of reasons for this: childcare duties may fall disproportionately to female patients in the home, or there could be different employment strains for women.
Q: Are the services patients receive for a telehealth visit of the same quality as an in-person visit?
Traditionally, in-person visits have included hands-on physical exams, such as taking a patient’s blood pressure or listening to a patient’s heart. With telehealth, one interesting thing is that we’re able to complete many of the same physical exam components. For example, you can use video to look at a patient’s legs for swelling or look at their neck for increased pressure. Right now, at our UPenn clinic, we’re creating care kits for patients to help with telehealth appointments. The kits may include a blood pressure monitor, an electronic stethoscope so we can listen to their heart, and other tools they can use at home. We can’t replicate every type of test, but there are many things we can do.
Q: What are some challenges of telehealth?
Using only a telephone without a video component makes it harder; it’s hard to always get a full understanding of the patient. However, a bigger challenge is that providers may not receive the same payment from insurers for telehealth services that they do for in-person visits, which may indirectly limit the use of telehealth services. Providers should have the flexibility to decide what type of visit is appropriate and not be penalized for selecting one appointment type over another.
Q: What are some of the benefits of telehealth services?
I find telehealth to be an incredible bonding experience overall. We get insight into patients’ lives, and they can see us in our home, too. I believe it provides more context and complete care for patients to see them in their home. For example, we can see the medicines patients are taking. Sometimes when a patient comes to the office, they may forget their prescriptions or may not remember how often they take it. With telehealth, patients can show me the bottles. Telehealth can help identify some safety or environmental barriers in the home, too. For example, some of my primary care colleagues have discovered that patients have rugs that are tripping hazards, which prompted them to suggest a home evaluation by a physical therapist.
Telehealth has also allowed for more involvement with family members. With in-person appointments, family members may not be able to attend because of work or other commitments. Telehealth makes us more accessible to families; they can ask questions or hear about care for the patient. We can also show results easily from different tests right on the screen.
Another huge benefit is with patients who are non-English-speakers. After seeing the disparities in telemedicine uptake among non-English speaking patients, we implemented an integrated real-time translator for visits. We’re able to click a button and a translator is immediately available by video as part of the visit. With in-person visits, we often have to wait for a translator to be available, which causes delay in care. The video translator program is so helpful that I now use it during in-person visits.
Finally, we can quickly complete care assessments outside of office hours. It allows us as providers to expand our normal hours. I can quickly talk to a patient at 7 p.m. on a Saturday about their blood pressure. I have found it can be quicker than coming into the office. I can spend more time talking to the patient and less time shuffling from patient to patient.
Q: We discussed how important it is to not just have technology, but to have the right technology.
Technology is important but every time we implement something new, I want us to ask ourselves how this tool or solution impacts equity. With this technology or solution, do all patients have equal access to the same care or information? After seeing disparities in telemedicine uptake, we at UPenn have tried to decrease barriers to connecting with the clinician via telemedicine. We’ve integrated text messaging into our telehealth appointment system whereby patients receive a text to join their appointment; they don’t have to download an app or other software. We can use the same text messaging system to tell patients whether a doctor is running late. Translation services are also integrated into the text messaging platform so instructions can be translated. This technology helps decrease some of the known barriers to telehealth.
Q: When is the right time to use telehealth versus an in-person appointment?
This depends on the patient’s diagnosis. For example, we can check blood pressure by video or phone quickly. Another option might be to evaluate all new patients in person and then transition them to telehealth appointments if appropriate for their specific medical issues. Giving providers the flexibility to make this choice with patients is helpful, which is why we strongly advocate for ensuring equal reimbursement from insurance for different types of appointments through permanent legislative action.
Q: What would you tell patients who are trying to decide between a telehealth visit and an in-person visit?
Patients have been nervous about in-person appointments because of COVID-19. However, we don’t want patients to put off their symptoms or questions; we want to intervene before patients get even sicker.
For patients wanting telehealth, I encourage them to connect with their clinic and providers to figure out what options are available. Opportunities for telehealth may vary greatly by specialty, clinic, and type of care.
*Originally published in The Beat – December 2021. Read the full newsletter here.



